Overview
Polycystic Ovarian Syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age. It causes irregular periods, excessive hair growth, acne, and weight gain due to an imbalance of hormones like insulin and androgens. Women with PCOS often have small fluid-filled sacs (cysts) on their ovaries, although not everyone with the condition develops these. PCOS can make it harder to get pregnant and may lead to long-term health issues like diabetes and heart disease if untreated. While the exact cause is unknown, genetics and lifestyle factors play a significant role. Treatment focuses on managing symptoms through medication, lifestyle changes, and healthy habits.
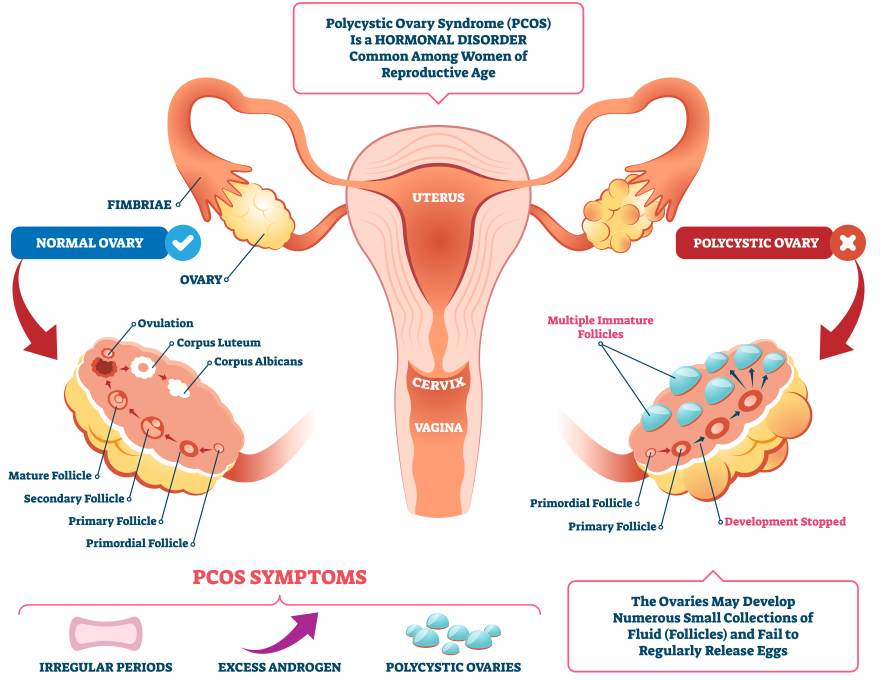
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting reproductive-aged women, characterized by multiple cysts on the ovaries, irregular menstrual cycles, and elevated androgen levels. It is a leading cause of infertility and is associated with various metabolic and cardiovascular risks.
1. Causes (Etiology):
The exact cause of PCOS is not fully understood, but several factors are believed to play a role:
• Genetics: A family history of PCOS increases the likelihood of developing the condition.
• Insulin Resistance: Insulin resistance and compensatory hyperinsulinemia contribute to increased androgen production, which leads to symptoms such as hirsutism and acne.
• Hormonal Imbalances:
• Elevated luteinizing hormone (LH) stimulates the ovaries to produce more androgens.
• Low levels of sex hormone-binding globulin (SHBG) increase the availability of circulating androgens.
• Obesity: Obesity exacerbates insulin resistance and hyperandrogenism, though PCOS can also occur in women of normal weight.
• Inflammation: Chronic low-grade inflammation is linked to higher androgen production.
2. Risk Factors:
• Family History: Women with a mother or sister with PCOS are more likely to develop the condition.
• Obesity: Being overweight or obese significantly increases the risk of developing PCOS.
• Insulin Resistance: A personal history of insulin resistance or Type 2 diabetes.
• Ethnicity: Women of South Asian descent are at higher risk and may present with more severe symptoms.
3. Pathophysiology:
• Hyperinsulinemia: High insulin levels reduce the liver’s production of SHBG, leading to increased free androgens in circulation. Insulin also directly stimulates the ovaries to produce more androgens.
• Hyperandrogenism: Excess androgen levels cause anovulation (absence of ovulation) and disrupt normal ovarian follicle development, leading to the formation of multiple cysts on the ovaries.
• Anovulation: Due to irregular or absent ovulation, women with PCOS experience irregular menstrual cycles and infertility.
• Metabolic Dysregulation: Insulin resistance increases the risk of metabolic complications such as Type 2 diabetes, dyslipidemia, and cardiovascular disease.
4. Signs and Symptoms:
• Menstrual Irregularities:
• Oligomenorrhea (infrequent periods) or amenorrhea (absence of periods).
• Hyperandrogenism:
• Hirsutism (excessive hair growth, especially on the face, chest, and back).
• Acne and oily skin.
• Alopecia (male-pattern hair thinning or hair loss).
• Infertility:
• Difficulty conceiving due to irregular ovulation or anovulation.
• Obesity and Weight Gain:
• Many women with PCOS struggle with weight gain, particularly around the abdomen.
• Acanthosis Nigricans:
• Dark, velvety patches of skin, often on the neck, armpits, or groin, indicating insulin resistance.
• Mood Disorders:
• Anxiety and depression are common, as well as issues with body image and self-esteem.
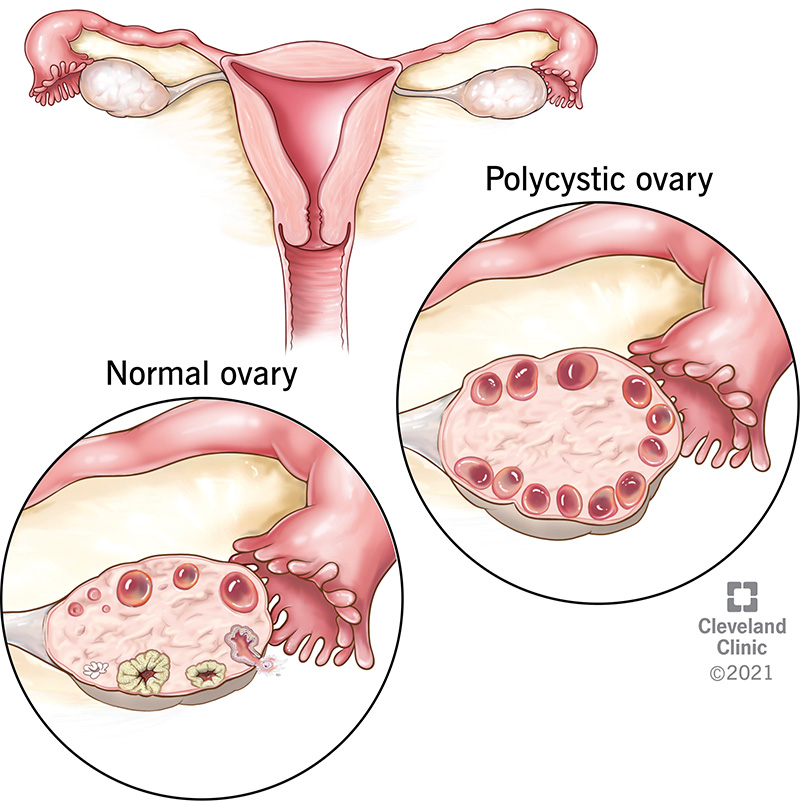
• Polycystic Ovaries:
• Enlarged ovaries with multiple small cysts (fluid-filled sacs).
5. Laboratory Investigations and Findings:
• Hormonal Levels:
• Increased LH/FSH ratio (usually >2:1).
• Elevated total testosterone and free testosterone levels.
• Elevated androstenedione and DHEAS (Dehydroepiandrosterone sulfate).
• Low SHBG.
• Normal or slightly elevated prolactin.
• Insulin and Glucose Levels:
• Elevated fasting insulin levels may indicate insulin resistance.
• Oral glucose tolerance test (OGTT): May reveal impaired glucose tolerance or Type 2 diabetes.
• Lipid Profile:
• Dyslipidemia is common, with low HDL (good cholesterol) and high LDL (bad cholesterol) or triglycerides.
• Pelvic Ultrasound:
• Shows enlarged ovaries with multiple small follicles (typically 12 or more in each ovary), giving a “string of pearls” appearance.
• Other Tests:
• Thyroid function tests and prolactin levels to rule out other causes of menstrual irregularities.
6. Treatment:
There is no cure for PCOS, but treatment focuses on managing symptoms and preventing complications. Treatment plans are often tailored based on whether the woman is trying to conceive.
• Lifestyle Modifications:
• Diet and Exercise: Weight loss (even 5-10%) can significantly improve symptoms, regulate menstrual cycles, and reduce insulin resistance.
• A balanced diet rich in whole grains, lean protein, and low in processed sugars helps regulate insulin levels.
• Medications:
• Oral Contraceptives (OCPs):
• Combined oral contraceptives are the first-line treatment for regulating menstrual cycles and reducing androgen levels.
• Anti-androgens:
• Spironolactone or finasteride may be prescribed to reduce androgen effects like hirsutism and acne.
• Metformin:
• Commonly used to improve insulin sensitivity and reduce blood sugar levels, particularly in women with insulin resistance or Type 2 diabetes. It can also help restore ovulation.
• Clomiphene Citrate (Clomid) or Letrozole:
• Used to induce ovulation in women trying to conceive.
• Gonadotropins or Assisted Reproductive Technologies (ART):
• Used when first-line ovulation induction treatments fail.
• Hair Removal:
• Laser hair removal or electrolysis can help manage hirsutism.
• Topical creams like eflornithine reduce facial hair growth.
• Surgical Intervention:
• Ovarian Drilling: A laparoscopic procedure that uses heat or laser to destroy small portions of the ovary to lower androgen levels and restore ovulation.
• Management of Metabolic and Cardiovascular Risks:
• Regular monitoring and management of blood glucose, lipids, and blood pressure.
• Preventive care to reduce the risk of Type 2 diabetes, cardiovascular disease, and endometrial cancer.
7. Complications:
• Infertility: Due to anovulation, PCOS is one of the most common causes of infertility.
• Type 2 Diabetes: Insulin resistance increases the risk of developing Type 2 diabetes.
• Endometrial Cancer: Chronic anovulation can lead to endometrial hyperplasia, increasing the risk of endometrial cancer.
• Obstructive Sleep Apnea: Women with PCOS, particularly those who are obese, have a higher risk of sleep apnea.
• Depression and Anxiety: Mood disorders are common in women with PCOS.
Frequently Asked Questions about Polycystic Ovarian Syndrome (PCOS)
- What is Polycystic Ovarian Syndrome (PCOS)?
PCOS is a hormonal disorder in women that affects the ovaries, causing irregular periods, excessive hair growth, acne, and potential fertility issues. - What causes PCOS, and is it genetic?
The exact cause of PCOS is unknown, but genetics, insulin resistance, and hormonal imbalances are significant contributors. - Can PCOS affect fertility?
Yes, PCOS can make it harder to conceive due to irregular ovulation, but treatments like lifestyle changes and medications can help improve fertility. - How is PCOS diagnosed?
PCOS is diagnosed through symptoms, blood tests to check hormone levels, and imaging tests like ultrasounds to detect ovarian cysts. - What are the best ways to manage PCOS?
PCOS management includes maintaining a healthy diet, regular exercise, weight management, and prescribed medications to balance hormones and address symptoms.