overview
Hypothyroidism is a condition where the thyroid gland doesn’t produce enough hormones to regulate the body’s metabolism, leading to symptoms like fatigue, weight gain, cold intolerance, and dry skin. Common causes include autoimmune disorders such as Hashimoto’s thyroiditis, iodine deficiency, and thyroid surgery. It is diagnosed through blood tests measuring TSH and T4 levels. Treatment involves daily thyroid hormone replacement, typically with levothyroxine, which helps restore normal hormone levels and alleviate symptoms. With proper management, people with hypothyroidism can live healthy, normal live.
Hypothyroidism is a condition where the thyroid gland doesn’t produce enough thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3). These hormones play critical roles in regulating metabolism, energy production, and overall body function.
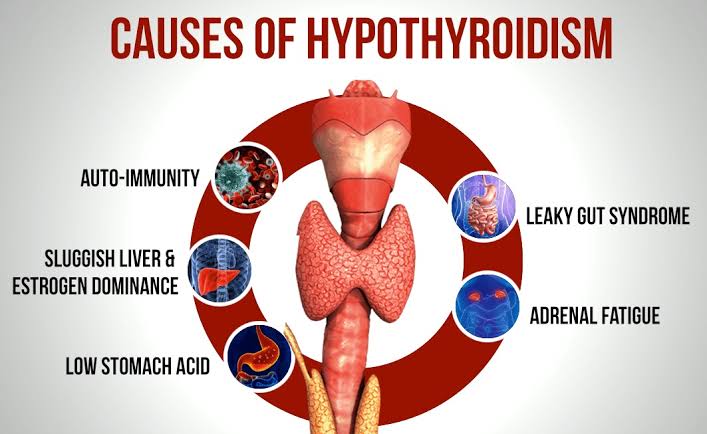
1. Causes (Etiology):
• Primary Hypothyroidism (most common):
• Hashimoto’s Thyroiditis: Autoimmune destruction of thyroid tissue.
• Iodine Deficiency: Low iodine intake impairs thyroid hormone production.
• Surgical Removal of the Thyroid: Thyroidectomy can lead to hypothyroidism.
• Radioactive Iodine Therapy: Used to treat hyperthyroidism but may damage the thyroid.
• Medications: Lithium, amiodarone, and anti-thyroid drugs can reduce thyroid hormone production.
• Secondary Hypothyroidism:
• Caused by pituitary gland dysfunction, leading to insufficient TSH (Thyroid Stimulating Hormone) production.
• Tertiary Hypothyroidism:
• Caused by hypothalamic dysfunction, where the hypothalamus fails to release TRH (Thyrotropin-releasing hormone).
2. Risk Factors:
• Gender: Women are more prone than men.
• Age: More common in individuals over 60 years.
• Family History: Genetic predisposition, especially for autoimmune causes.
• Previous Thyroid Problems: History of thyroid surgery or radiation therapy.
• Iodine Deficiency or Excess: Too little or too much iodine can interfere with thyroid function.
• Autoimmune Disorders: Conditions like Type 1 diabetes, celiac disease, or lupus increase risk.
3. Pathophysiology:
• Inadequate Thyroid Hormones: Reduced levels of T3 and T4 lead to a decreased metabolic rate.
• Compensatory TSH Elevation: In primary hypothyroidism, the pituitary releases more TSH in an attempt to stimulate the thyroid, resulting in high TSH levels.
• System-wide Impact: Hypothyroidism affects multiple systems, causing slower metabolism, altered cardiac output, gastrointestinal motility issues, and impaired growth and development (in children).
4. Signs and Symptoms:
• General: Fatigue, weight gain, cold intolerance, and lethargy.
• Skin: Dry, rough, pale skin; coarse hair; hair loss.
• Cardiovascular: Bradycardia (slow heart rate), low blood pressure, and high cholesterol.
• Gastrointestinal: Constipation.
• Neurological: Depression, memory impairment, and difficulty concentrating.
• Reproductive: Menstrual irregularities and infertility.
• Myxedema: Severe cases lead to non-pitting edema in the skin (especially face and limbs).
• Goiter: In some cases, thyroid gland enlargement may occur.
5. Laboratory Investigations and Findings:
• Serum TSH:
• Elevated in primary hypothyroidism (compensatory mechanism).
• Low or normal in secondary or tertiary hypothyroidism.
• Free T4:
• Low in all forms of hypothyroidism.
• Free T3:
• Usually normal or low.
• Thyroid Antibodies:
• Anti-thyroid peroxidase (Anti-TPO) and anti-thyroglobulin antibodies are often elevated in autoimmune hypothyroidism (Hashimoto’s thyroiditis).
• Cholesterol levels: Often elevated, reflecting slowed metabolism.
• CBC: May show anemia, typically normocytic or macrocytic.
• Imaging:
• Thyroid ultrasound: To assess for nodules or gland enlargement.
• Radioactive iodine uptake test: Decreased uptake in primary hypothyroidism.
6. Treatment:
• Thyroid Hormone Replacement:
• Levothyroxine (Synthetic T4) is the standard treatment. It is administered orally and adjusted based on regular monitoring of TSH and T4 levels.
• Goal: Normalize TSH levels and alleviate symptoms.
• Iodine Supplementation (for iodine deficiency cases).
• Addressing Underlying Causes: If medication-induced, adjustment or discontinuation of the offending drug might be needed.
• Monitoring:
• Regular follow-ups to adjust levothyroxine dosage based on TSH and T4 levels.
• Special attention in pregnancy
